The arrival of the Paramedic
As previously referenced it was the 1948 Health Act from which the ambulance service was born. It was a weak and tottering service, full of mistakes, but nevertheless, a service that was to become the envy of the free world. In its early years the importance of the role that ambulance staff could play, in relation to what we now know as the chain of survival, was not understood or appreciated in civilian life. This was despite massive experience and evidence being gained in the battlefields of world war 2 certainly in relation to the control of haemorrhage, fluid replacement and pain relief.
It would be a further 26 years before the total responsibility for the ambulance service fell under the National Health Service. Moving the Ambulance Service under the umbrella of the NHS would ultimately help launch and shape the modern paramedic.
It would be a further 26 years before the total responsibility for the ambulance service fell under the National Health Service. Moving the Ambulance Service under the umbrella of the NHS would ultimately help launch and shape the modern paramedic.
In 1950 the ambulance equipment consisted of a stretcher, basic splinting packs, bandages and oxygen therapy. People started to appreciate the benefits of first aid and the new teams wanted better skills and equipment. In the early 80's things had progressed for the better in that oxygen units such as the minuteman, entonox pain relief and scoop orthopaedic stretchers were standard items of equipment but there was still key equipment lacking. Role specific cervical collars were not there, staff still used brooks airways and good aspiration/suction equipment was not on every vehicle.
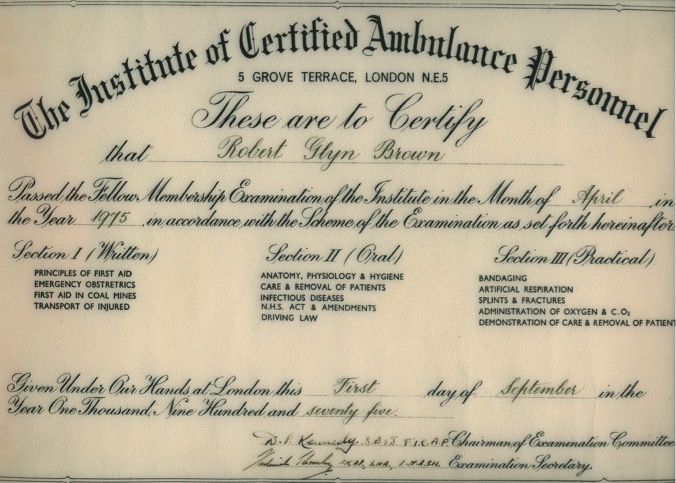
Institute of Certified Ambulance Personnel
In 1948, originating in the South of England the Institute of Certified Ambulance Personnel (ICAP) was formed. This was a voluntary organisation, which brought doctors and ambulance men together in their quest for better training and equipment. The curriculum was relevant, forward thinking and importantly paid cognisance to the impact ambulance staff could make in the patients chain of survival. The course content covered a high level of anatomy and physiology, medical and trauma conditions, management of illness and injury, obstetrics and gynaecology, NHS Law and driving regulations. There were two awards levels of Associate and Fellow and driven by self study; Ambulance Training standards began to improve and their importance recognised.
Of great benefit for the Liverpool Area was that the Chief Albert Guinney was a great advocate of ICAP and the future Ambulance Service Institute examinations and actively promoted their take up within his Ambulance Team. When he started his Cadet Force in 1964 all Cadets were put through the ICAP/FASI Qualifications which would ultimately benefit the future paramedic schemes.
Of great benefit for the Liverpool Area was that the Chief Albert Guinney was a great advocate of ICAP and the future Ambulance Service Institute examinations and actively promoted their take up within his Ambulance Team. When he started his Cadet Force in 1964 all Cadets were put through the ICAP/FASI Qualifications which would ultimately benefit the future paramedic schemes.
A long Journey
Recognition is given that these shoots of budding paramedic ambition was being driven by the Chief Albert Guinney whose vision for improving ambulance aid had its roots in 1960 when he took up his position.
Nationally, there were some early adopter Paramedic Schemes such as in Brighton and also in London where we started to see the rollout of Infusion and Intubation Crews.
Locally; Peter Hanton began training under the guidance of Doctor Allan of Broadgreen Accident and Emergency Unit. Peter would receive training in intubation and infusion but the delivery of actual Paramedic Care on the streets of liverpool would have to wait until the arrival of the IHCD National Qualification in 1986.
A fact that is easy to forget, given the availability of modern day commonplace technology, is that in the early 1980's the battery charged portable defibrillator was simply not there. Battery technology was in its early stages and the batteries to operate a portable defibrillator were huge. They were also very expensive. When Merseyside Ambulance deployed its first defibrillator (Cardiac Recorders CR26) in 1986 staff will tell you how difficult it was to carry because of its sheer weight.
Nationally, there were some early adopter Paramedic Schemes such as in Brighton and also in London where we started to see the rollout of Infusion and Intubation Crews.
Locally; Peter Hanton began training under the guidance of Doctor Allan of Broadgreen Accident and Emergency Unit. Peter would receive training in intubation and infusion but the delivery of actual Paramedic Care on the streets of liverpool would have to wait until the arrival of the IHCD National Qualification in 1986.
A fact that is easy to forget, given the availability of modern day commonplace technology, is that in the early 1980's the battery charged portable defibrillator was simply not there. Battery technology was in its early stages and the batteries to operate a portable defibrillator were huge. They were also very expensive. When Merseyside Ambulance deployed its first defibrillator (Cardiac Recorders CR26) in 1986 staff will tell you how difficult it was to carry because of its sheer weight.
Association of Emergency Medical Technicians.
Staff wanted things to change and were watching what was happing in America with the development of the paramedic which had been greatly influenced by the battlefield care delivered by medics in the Vietnam war. Steve Noonan, Ray Lunt and Mike Jackson formed a local branch of an organisation know as the Association of Emergency Medical Technicians (AEMT) which had the aim of improving the education of staff to help them become paramedics. Inspirational and thought provoking lectures were arranged which helped get the Medical profession on board and through study people raised their standards.
The great Paramedic Magazine JEMS was subscribed to and each journal brought exciting research and ambition through researched articles. The budding paramedic bible became Nancy Carolines "Emergency Care on the Streets" and ECG strips began to be studied.
The great Paramedic Magazine JEMS was subscribed to and each journal brought exciting research and ambition through researched articles. The budding paramedic bible became Nancy Carolines "Emergency Care on the Streets" and ECG strips began to be studied.

The first Paramedic Cohort - National Institute Health Care Development IHCD) - Extended Training Qualification
National Curriculums were developed and in 1985 the IHCD Extended Training Qualification was launched. Entrance examinations were undertaken and selection panels sat consisting of A & E Consultants and Cardiologists. These great doctors formed what was known as the Local Ambulance Advisory Panel and became the oversight body for sponsoring the Paramedic Scheme in Merseyside putting their professional weight being getting the scheme launched.
The first paramedic cohort (who have all now retired) were Dave Buckley, Ray Lunt, Ken Morgan and Steve Noonan. After successfully completing their National Examinations they completed 3 months intensive training in the Royal Liverpool (Ray and Steve) and Arrowe Park Hospitals (Dave and Ken).
Behind the great initiative was the weight, support and guidance of some very eminent and visionary doctors such as Dr Lawrence Jaffey, Dr Jonathan Marrow, Dr Raymond Ahern and Dr Rodrigues to mention a few.
It was spring 1986 when the first cohort of Paramedics went live on the streets of Liverpool with their personal issue Ambu Resuscitation Cases and Cardiac Recorders CR26 defibrillators. In the early days they simply staffed their normal ambulances but added the word Delta to the call sign which indicated the presence of a paramedic. It was hard to provide area cover 24/7 with just 4 paramedics so a decision was made to move the paramedics on to what became the first rapid response vehicle Whisky Delta One which operated centrally from Anfield Station which was alongside the Control Room. Whisky Delta One had great success in that it allowed the paramedics to target the bad cases of cardiac arrest, RTC entrapments and major trauma. It also had a fantastic motivational effect on inspiring the next cohorts of paramedics that were required to grow the scheme so that more patients would benefit from receiving paramedic care in their hour of need.
The first paramedic cohort (who have all now retired) were Dave Buckley, Ray Lunt, Ken Morgan and Steve Noonan. After successfully completing their National Examinations they completed 3 months intensive training in the Royal Liverpool (Ray and Steve) and Arrowe Park Hospitals (Dave and Ken).
Behind the great initiative was the weight, support and guidance of some very eminent and visionary doctors such as Dr Lawrence Jaffey, Dr Jonathan Marrow, Dr Raymond Ahern and Dr Rodrigues to mention a few.
It was spring 1986 when the first cohort of Paramedics went live on the streets of Liverpool with their personal issue Ambu Resuscitation Cases and Cardiac Recorders CR26 defibrillators. In the early days they simply staffed their normal ambulances but added the word Delta to the call sign which indicated the presence of a paramedic. It was hard to provide area cover 24/7 with just 4 paramedics so a decision was made to move the paramedics on to what became the first rapid response vehicle Whisky Delta One which operated centrally from Anfield Station which was alongside the Control Room. Whisky Delta One had great success in that it allowed the paramedics to target the bad cases of cardiac arrest, RTC entrapments and major trauma. It also had a fantastic motivational effect on inspiring the next cohorts of paramedics that were required to grow the scheme so that more patients would benefit from receiving paramedic care in their hour of need.

Whiskey Delta One - First bespoke designed RRV (2.9i 4 x 4 Ford Sierra)
We knew it was only a matter of time before our Paramedic skills were used in anger. I was the first Paramedic to defibrillate a patient on the actual streets of Liverpool. Both Toxteth crews myself Bobby Graham, Bob Poynton and George Mitchell attended a cardiac arrest call for a member of the Orange Lodge band who had collapsed in Leece Street. You have to relate to the fact that no-one had ever seen anyone be defibrillated in a pre-hospital setting before; so when we screamed up and jumped out of the sliding doors of the ambulances (in those days); it was an eye opener for the other emergency services and public alike. We were so pleased, relieved and proud that the training kicked in and we managed to get a succesful return of spantaneous circulation to a round of applause from the crowd. We all knew at that time that out of all the skills we now had it would be defibrillation that would make the greatest survival difference and it greatly pleases me to see how available the AED is nowadays.
Ray Lunt
-

Dave Buckley
-

Ray Lunt
-

Ken Morgan
-

Steve Noonan
Heartstart
There were many obstacles to getting the Merseyside Paramedic Scheme off the ground. There were a lot of non-believers who believed the Ambulancemen and Ambulancewomen were simply not up the mark to being able to intubate, infusion and administer drugs. Another major hurdle was that of funding to buy the paramedic equipment of resuscitation cases and defibrillators. In 1987 Paul Townley and Steve Eyre formed a local charity called heartstart with an inspirational goal of raising enough equipment to make sure that all ambulances in Merseyside were equipped with life saving defibrillators. A sterling effort by Paul and Steve along with great public support saw that by the early 90's every Merseyside Ambulance was equipped with a defibrillator. The Heartstart scheme has continued to this day.
At the beginning of the Paramedic Scheme Training it was appreciated early on that it would time to train Paramedics and opportunities were being missed to deliver defibrillation to all cardiac arrest victims. A stepping stone was introduced in the form of a defibrillation course which enabled us to quickly get to the point in which it started become unthinkable that any cardiac arrest victim in Merseyside would not get a defibrillator to them with the first responding crew.



